In an effort to improve operational efficiency, information flow and quality of care, area healthcare facilities are increasing their use of electronic health record systems (EHRs).
“There’s been a significant move to automate as many clinical processes as possible,” said Dr. Jay Eisenberg, chief medical information officer at Vancouver’s PeaceHealth Southwest Medical Center.
Eisenberg said PeaceHealth Southwest added a computerized provider order entry module to their EHR in July. The roll-out involved training 1,100 nurses, 800 physicians, and 200-300 ancillary care givers such as pharmacists and therapists.
A growing trend
EHRs are not a new thing – they have existed in some form since the 1960s. But as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009, Congress has approved incentives and penalties to speed EHR adoption.
Incentives range from $44,000 to $65,000 per physician. Penalties will take the form of decreased Medicare and Medicaid reimbursements to doctors who fail to use EHRs by 2015. A 2009 study conducted by the U.S. Centers for Disease Control (CDC) reported that the EMR adoption rate rose from 38.4 percent in 2008 to 48.3 percent in 2009.
Eisenberg said that PeaceHealth Southwest has used an EHR – the McKesson system – for several years. Other PeaceHealth hospitals use a GE-based product, while PeaceHealth’s ambulatory clinics are converting to the Epic system over the next two years.
Cheryl Forry, nurse manger of the ICU at Legacy Salmon Creek Medical Center, said that Legacy Salmon Creek has also recently converted to Epic – the same system used by Vancouver Clinic, Providence, Kaiser Permanente and OHSU.
Information access
Forry said that EHRs can help with patient safety, such as reducing errors associated with illegible physician handwriting. Also, she said, if properly integrated, they can provide better access to patient information and better efficiency. For example, if a patient is admitted from the emergency room, in-patient doctors could access the data gathered by the ER.
However, integration is an ongoing challenge. Dr. Don Benz, an independent physician in Vancouver, has used an EHR for more than eight years. Yet, when one of his nurse practitioners transferred to a different clinic that used the same EHR, he would have had to pay $24,000 for an interface between his system and the other clinic’s in order to transfer the nurse practitioner’s files electronically.
“Even having the same vendor does not guarantee seamless flow of information back and forth,” said Eisenberg. “We’re not there yet.”
Teaching old dogs new tricks
Forry said that when Legacy Salmon Creek opened in 2005 with their original EHR, most staff disliked it, finding it time consuming. But now, she said, most staff prefer the EHR to using paper-based processes.
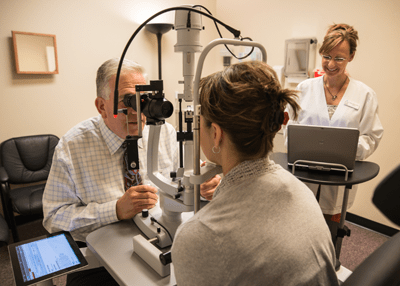
When installing or converting an EHR, organizations use a combination of vendor-supplied on- and off-site training and webinars. Additionally, Forry said that some of Legacy’s staff became vendor-certified “tutors” who provided several weeks of at-the-elbow training to other staff members. Dr. Richard Bernheimer, president of Eye Care Specialists of Vancouver, said some of his staff serve as “experts” on various EHR modules.
Counting the cost
Benz said his EHR system initially cost $50,000, and he pays $600 per quarter for scheduled updates. Additional changes, such as adding the whooping cough vaccine to the system, cost extra. Bernheimer said his initial implementation costs were about $7,500; monthly costs are about $2,000. Bernheimer’s system handles billing as well, which costs 5 to 8 percent of collections.
“For big organizations or individual practices,” said Eisenberg, “the cost is not inconsequential.”
On-premise systems typically require costs for licenses, servers, implementation, training and ongoing technical support. Support costs are typically 15 to 20 percent of the upfront licensing cost per year. Implementation and training costs also vary widely, but are often as high as the licensing costs.
Bernheimer pointed out that EHRs typically also mean increased hardware costs, since each staff member typically has a tablet or other small-form factor device for accessing the system.
A work in progress
Benz said that he and many of his colleagues find EHRs to be cumbersome.
“They are not designed to think like a physician thinks,” said Benz. “[EHRs] don’t give the nuances of a patient’s condition like a written record does. Simply printing can take six or seven mouse clicks.”
A 2009 study by the Healthcare Information and Management Systems Society, a large U.S. healthcare IT industry trade group, observed that EHR adoption rates “have been slower than expected in the United States. A key reason, aside from initial costs and lost productivity during implementation, is lack of efficiency and usability.”
Forry said that during the first few weeks of the roll-out, a “Top 10 at 10” forum met at 10:00 a.m. every morning to identify and prioritize design flaws – the top ten problems were to be fixed by that evening.
“We’re continuing that same process as we roll out Epic at Legacy locations in Oregon,” said Forry.
Reliability and security are also concerns. Benz uses dual hard drives and performs a daily tape and external hard drive backup. In contrast, Bernheimer’s EHR is cloud-hosted. But outages do occur. For example, dozens of hospitals across the country lost access to crucial electronic medical records for about five hours during a major computer outage on July 23.
Although EHRs could reduce inadvertent exposure of medical information, Benz said, they made it easier for hackers to access large amounts of data at once. It takes far less time to obtain a username and password than it does to make copies of paper charts.
“In the healthcare industry,” said Bernheimer, “the evolution of computer use is behind where it is in other industries.” He opined that privacy and data integrity concerns were a major contributing factor. But, he said, to provide the highest quality of care, these problems must be overcome.
“The future is that we will have to integrate and share all health data,” said Bernheimer. “Data has to be accessible and transferrable.”
Implementing an Electronic Health Record (EHR)
According to Dr. Jay Eisenberg, chief medical information officer at PeaceHealth Southwest Medical Center, deploying an EHR is not a walk in the park.
“It’s a very big disruptive change for organizations to do this,” said Eisenberg. “It’s a transformation of work flows and order management. It requires a lot of support and careful attention to detail.”
The following guidelines from HealthIT.gov can help practitioners make the transition to an EHR:
- Assess practice goals, needs, and financial and technical readiness.
- Plan for HER implementation, using the information gathered in step 1.
- Select or upgrade to a Certified EHR to achieve meaningful use and qualify for incentive payments.
- Install the EHR system, and conduct training and pilot testing.
- Successfully attest to demonstrating meaningful use of EHRs, and reassess what you have learned from training and daily use of the system.
- Continuously evaluate your practice’s goals and needs to improve workflows and leverage the functionality of the EHR system.